Liver Awareness Month: Fibrosis
Let’s Stop the Progression of Liver Disease
Last week, in our hepatitis blog post, we reviewed the role of inflammation in the liver and what happens when someone has liver disease and develops hepatitis.
As a refresher, inflammation occurs when a healthy liver is hard at work destroying toxins or invaders and repairing damaged cells. Damaged liver cells and immune cells both send out messages to activate specific repair cells which travel to the site of the injury. These repair cells release something called collagen, a fiber, which stiffens the tissue around the cells, protects the surviving cells, and allows healing to occur. In a healthy liver, this repair process is very closely regulated and, when no longer needed the extra collagen will disperse and the liver returns to normal.
When someone has liver disease, their liver enters into a very dangerous cycle. Persistent inflammation, or hepatitis, sends nonstop signals to the repair cells to continue depositing collagen. The extra collagen stiffens around the tissue like it is supposed to in the healthy liver; but, instead of a signal being released to stop the inflammation and discard the extra collagen, the inflammation continues, and even more collagen is deposited, leading to more stiffening. This is how fibrosis develops.
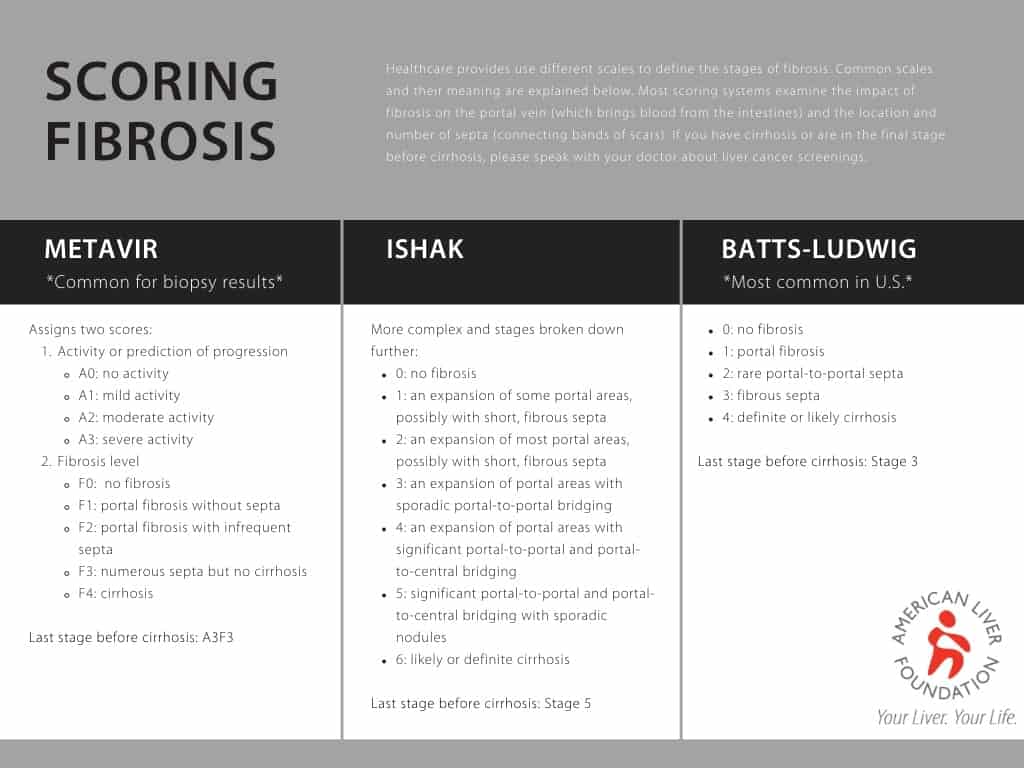
When repetitive damage or long-lasting inflammation occurs, collagen and other proteins build-up between liver cells, forming scar tissue. Scar tissue can block or limit blood flow within the liver, starving and killing healthy liver cells, causing more scar tissue to form. Unlike healthy liver cells, scar tissue cannot function or repair itself. As fibrosis advances it can impact the liver’s ability to function, limit its ability repair itself, and restrict blood flow. Over time, the scars in the liver will continue to build and replace healthy tissue. Gradually, the scars snake out further, covering more of the healthy liver and grow together, or bridge, creating septa or bands of scar tissue. Fibrosis also restricts blood flow; when a doctor wants to determine how severe the scarring is, they examine the impact on the portal blood flow (the portal vein brings all the blood from the intestines to the liver to be processed).
Fibrosis in mild to moderate stages often does not cause symptoms. Due to a lack of symptoms, many people live with liver damage, or fibrosis, without being diagnosed until they have symptoms of cirrhosis. Fibrosis can be reversed if detected early enough and the underlying liver disease that caused the development of fibrosis can be cured or treated. If fibrosis is left untreated, it can lead to cirrhosis and liver cancer. It is important to remember that the process of fibrosis progressing to cirrhosis happens over a long period of time. The time it takes for fibrosis to progress is different for every disease and every person. Not everyone who develops fibrosis will progress to cirrhosis. Not everyone who gets cirrhosis will get cancer.
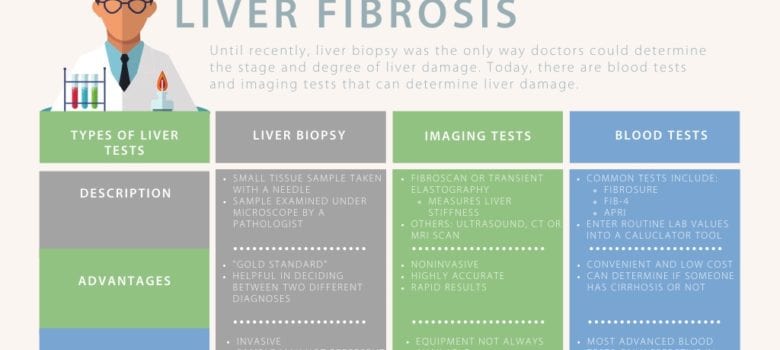
If you have been diagnosed with liver disease, it is important to know the stage of your liver damage. Knowing the stage of your liver disease will impact the decisions you and your care team make about your health. People with more advanced fibrosis or cirrhosis will need to receive surveillance for liver cancer, may need to avoid certain medications, and may need to be seen by their doctor more frequently for blood tests. There are several tests that can diagnose liver damage. There are also a few scoring systems used. Learn more about them below.
American Liver Foundation is solely responsible for this content, which is made possible through generous support from Mallinckrodt and Salix.
As a reminder, fibrosis is the process of scar tissue building up in the liver, replacing healthy functioning cells, and causing stiffening or hardening of the liver which reduces blood flow. The final stage of fibrosis is cirrhosis. Cirrhosis is where your liver is severely scarred and permanently damaged. While the word cirrhosis is most commonly heard when people discuss alcohol-induced liver disease, cirrhosis is caused by many forms of liver disease.
When we talk about cirrhosis, it’s important to remember that there is a big difference between liver functioning and disease progression. Our livers are resilient, continuing to function even when they become severely scarred; because of this, some people may not experience symptoms or have elevated liver enzyme tests even though their liver is damaged. It is important to talk to your doctor about your risks for liver disease so you can receive imaging tests that may help diagnosis liver damage.
When someone has cirrhosis, their liver shrinks and becomes hard, greatly impacting the liver’s ability to process the massive amounts of blood for which it’s responsible. Did you know the liver’s biggest role is to filter our blood all day, every day? At any given moment, your liver contains about a pint, or 13% the body’s total blood supply; the liver filters more than a liter of blood every minute which is about 22 gallons of blood per hour and more than 250 gallons of blood in a 24-hour time period. There are two sources that supply all this blood to the liver: the hepatic artery and the hepatic portal vein. The hepatic artery brings oxygen-rich blood into the liver. Blood coming from our digestive system enters the liver through the hepatic portal vein carrying nutrients, medications, or toxins.
Last updated on August 4th, 2022 at 04:39 pm