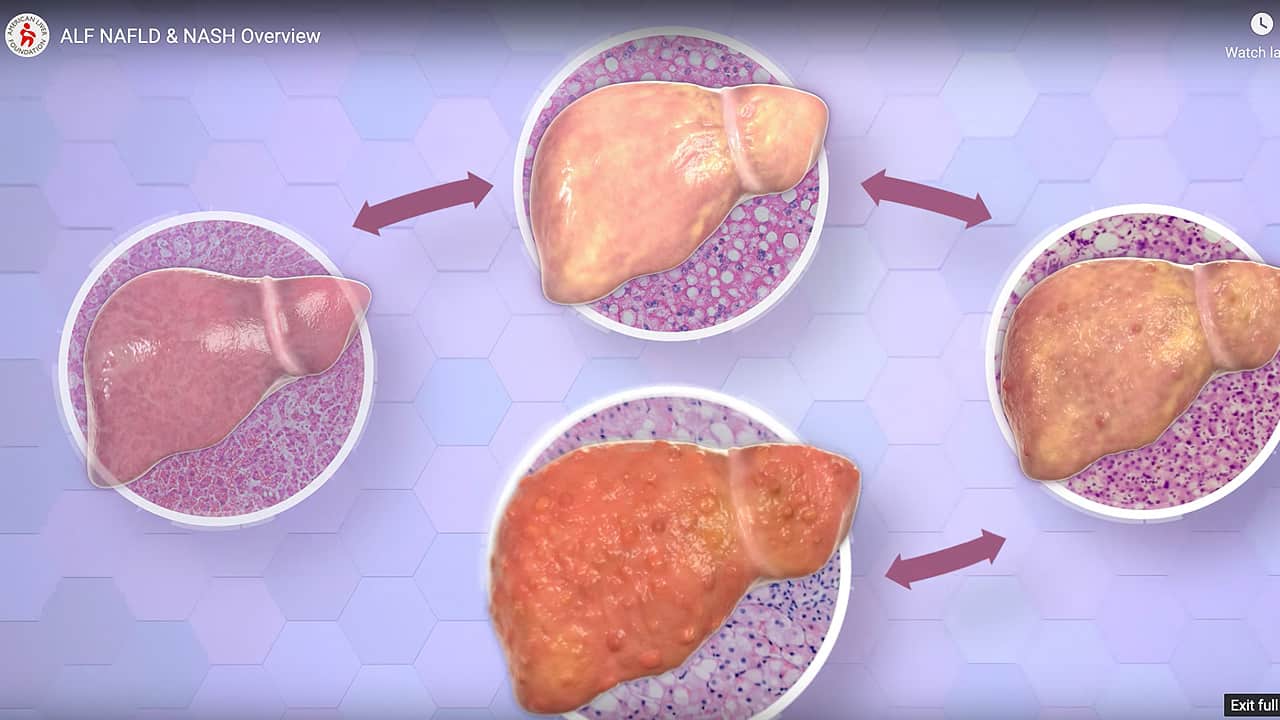
Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD)
Overview
Metabolic dysfunction-associated steatotic liver disease, or MASLD, is the buildup of extra fat in liver cells that is not caused by alcohol. MASLD had been previously called NAFLD, or nonalcoholic fatty liver disease. It is normal for the liver to contain some fat. However, if more than 5% – 10% percent of the liver’s weight is fat, then it is called a fatty liver (steatosis).
The more advanced form of MASLD is MASH (metabolic dysfunction-associated steatohepatitis). MASH used to be known as NASH, or nonalcoholic steatohepatitis. MASH causes the liver to swell and become damaged.
We encourage adults living with MASH/NASH to visit our MASH Featured Clinical Trial page to learn more about potential opportunities in their area. Visit the page today.
Finding out you have MASLD can be daunting, but watch how Shawanna met the challenge head on and is reversing her diagnosis with weight loss, healthy eating and exercise!
Facts at-a-Glance
- About 100 million people (about 25%) in the United States are estimated to have MASLD (previously called NAFLD).
- MASLD is the most common form of liver disease in children and has more than doubled over the past 20 years.
Symptoms and Causes
Learn more about MASLD/MASH with this print-friendly infographic.
Metabolic dysfunction-associated steatotic liver disease, or MASLD (formerly called NAFLD) tends to develop in people who have increased body fat or have diabetes, high cholesterol, or high triglycerides. Having a combination of these conditions is known as metabolic syndrome. Rapid weight loss and poor eating habits also may lead to MASLD. Certain medications may increase one’s chances of developing MASLD. It is important to note, however, that some people develop fatty liver even if they do not have the most common risks.
What is the MASLD/heart health connection?
Metabolic dysfunction-associated steatotic liver disease (MASLD, formerly known as NAFLD) and cardiac (heart) disease have similar causes, including metabolic syndrome. Metabolic syndrome is a grouping of health conditions that include high triglycerides, high blood sugar levels, prediabetes and Type 2 diabetes, and high blood pressure. Other factors include obesity and excess fat around the abdomen (belly area).
Current medical recommendations suggest the importance of discussing the MASLD/heart disease connection with a health care provider if you have MASLD. Although you may be worried about your liver health, death from cardiovascular disease (CVD) is more common than liver complications among people with fatty liver. Even if the fatty liver disease progresses to significant fibrosis (scarring in the liver that is cirrhosis or nearly cirrhosis), the risk of CVD remains higher than the risk of liver complications
What happens if MASLD gets worse?
Metabolic dysfunction-associated liver disease (MASLD), formerly called NALFD, can get worse and cause liver inflammation (enlargement or swelling) and damage called metabolic dysfunction-associated steatohepatitis, or MASH. MASH used to be known as NASH, or nonalcoholic steatohepatitis. Over time, inflammation can lead to scarring in the liver and progress to a irreversible buildup of scarring, known as cirrhosis. Early diagnosis of MASLD, along with following medical advice, can reduce a person’s chance MASLD progressing to MASH and cirrhosis.
What are the symptoms of MASLD and MASH?
MASLD (formerly called NAFLD)) often has no symptoms. If symptoms begin, however, they usually include fatigue (extreme tiredness), weakness, discomfort or pain in the abdomen.
If MASLD begins to advance to MASH (formerly known as NASH), other symptoms may begin. These can include jaundice (yellowing of the eyes and skin), severe itching, fluid buildup in the belly (ascites) and fluid buildup in the ankles (edema). Sometimes mental confusion can occur.
What about MASLD and Pregnancy?
While MASLD (formerly called NAFLD) can affect people of all ages, sexes, and ethnicities, it is important to consider its specific implications during pregnancy and in those intending to become pregnant. MASLD affects about 18% of pregnant women, and pregnancy can exacerbate existing MASLD due to normal hormonal changes, largely by increased estrogen, and the natural insulin resistance of pregnancy.
The risk factors for developing MASLD during pregnancy are similar to times outside of pregnancy, and include obesity, pre-existing diabetes, prior gestational diabetes, and advanced maternal age. Being diagnosed with MASLD prior to pregnancy is associated with an increased risk of developing gestational diabetes, hypertensive complications such as pre-eclampsia, preterm birth, adverse fetal outcomes, and childhood development of obesity and MASLD in the offspring. Diagnosis typically involves ultrasonography after investigation for other causes of elevated liver enzymes.
Once MASLD is determined, management of the condition focuses on lifestyle interventions (health dietary modifications and appropriate physical activities permitted during pregnancy) as there are no approved medications for MASLD in pregnancy. Prior to pregnancy, preconception counseling, weight management, and optimal blood sugar control are important measures for preventing the development or progression of MASLD. Importantly, breastfeeding may reduce MASLD risk for both the mother and their child. Ultimately, close monitoring during pregnancy is crucial to reduce risks and improve outcomes for both the mother and her child. Download a fact sheet about MASLD (NAFLD) and pregnancy.
Diagnosis and Tests
MASLD may be suspected if blood tests show higher than normal levels of liver enzymes. Usually, doctors will have to rule out other probable causes of higher-than-normal liver enzymes before they know for sure if someone has MASLD. It is important to understand that some people have MASLD even if their liver enzyme levels are within normal range. Doctors will review a person’s medical history and will often order additional tests such as ultrasound, which can show what the liver looks like, to see if anything looks abnormal.
Management and Treatment
Eating a healthy diet and adding physical movement to your day may help prevent liver damage from starting or reverse it in the initial stages. Here are suggestions for people who have MASLD:
- See a liver specialist (gastroenterologist or hepatologist) to monitor and advise you about your liver health.
- If you are overweight or obese, speak to your doctor or a dietitian to learn more about planning healthy meals that can help you lose weight.
- If you have high cholesterol or high triglycerides, speak with your doctor about how to lower your numbers to a healthier range.
- If you have diabetes, speak with your doctor about managing your condition.
- Avoid alcohol (beer, wine, hard liquor) to lower the risk of additional liver damage.
There are some new treatments that may help people with MASLD, so it is important to discuss whether these medications may be appropriate for you if you have been diagnosed with this disease.
Prevention
There are things people can do to lower their chances of developing MASLD (previously called NAFLD). They include:
- Maintain a healthy weight.
- Eat meals that contain lean proteins, whole grains, fruits, vegetables, healthy oils, and low-fat dairy products.
- Try to include some kind of physical movement during most days of the week. If you are not currently physically active, speak with your doctor about the types of activities you can do that are safe for your current physical abilities.
- Limit or avoid alcohol intake.
- Only take medicines that you need, and follow dosing recommendations.
Outlook and Prognosis
The outlook for people with MASLD depends upon how advanced the condition has become. People with early stages of MASLD who work closely with their doctors can do very well for many years, in some cases reversing the condition. Others with more advanced liver damage associated with MASH are at higher risk for developing cirrhosis (scarring) of the liver and primary liver cancer (hepatocellular carcinoma).
Anyone with MASLD or MASH should be in the care of a liver specialist (gastroenterologist or hepatologist) and follow doctors’ recommendations for lab work, ultrasound, or liver scans to monitor their health.
Living with MASLD
People who have been diagnosed with MASLD are advised to follow the recommended schedule for doctor visits and tests. If possible, consider speaking with a dietitian or nutritionist who can provide helpful information about healthy eating options. Physical activity may also be of benefit, so speak to the doctor to make sure that you can begin an exercise program safely.
Questions to Ask Your Doctor
- What condition do I have that suggests MASLD (previously referred to as NAFLD)?
- Can MASLD (NAFLD) be reversed? How long can this process take?
- Do I have fibrosis or cirrhosis (early or advanced scarring of the liver?
- If I have cirrhosis, how advanced is it?
- What kinds of dietary and lifestyle changes do you suggest that I make?
- Can you refer me to a registered dietitian or nutritionist to help me plan healthy meals?
- What kinds of physical activities would be OK for me to do?
- Is there a treatment or medication for MASLD? Are there any clinical trials that might be good for me?
- Is there a treatment or medication for MASH? Are there clinical trials that might be good for me?
- Will losing weight reverse this disease and help my liver go back to full health?
Support Group
MASH (previously called NASH) Support Group on Facebook
Visit the American Liver Foundation dysfunction-associated steatosis (MASH) (formerly called NASH, or nonalcoholic steatosis) support group on Facebook. For more details, click here…
Clinical Trials
We encourage adults living with MASLD to visit our Clinical Trials page to learn more about opportunities in their area. Visit our Clinical Trials page today.
New Nomenclature (Name) of NAFLD
MASLD, or metabolic dysfunction-associated liver disease, is the new name of NAFLD (nonalcoholic fatty liver disease) Learn about the new nomenclature (terminology) changes here.
Video Library
Patient Stories
Search for a Clinical Trial
Clinical trials are research studies that test how well new medical approaches work in people. Before an experimental treatment can be tested on human subjects in a clinical trial, it must have shown benefit in laboratory testing or animal research studies. The most promising treatments are then moved into clinical trials, with the goal of identifying new ways to safely and effectively prevent, screen for, diagnose, or treat a disease.
Speak with your doctor about the ongoing progress and results of these trials to get the most up-to-date information on new treatments. Participating in a clinical trial is a great way to contribute to curing, preventing and treating liver disease and its complications.
Start your search here to find clinical trials that need people like you.
Medically reviewed on April 2025.
Last updated on September 25th, 2025 at 03:38 pm