Hepatocellular Carcinoma
Know the risks and understand the symptoms of Hepatocellular Carcinoma
Get screened and talk to your doctor today about Hepatocellular Carcinoma treatment alternatives.
Cancer is the growth and spread of unhealthy cells in the body.
Primary liver cancer is a type of cancer that starts in the liver. Other names for primary liver cancer are hepatoma or hepatocellular carcinoma (abbreviated as HCC).
Secondary liver cancer is a type of cancer that starts somewhere else in the body and spreads to the liver. The medical term for a cancer that has spread is metastatic, so secondary liver cancer is also referred to as metastatic liver cancer.
Hepatocellular carcinoma is the most common type of cancer among adults in the USA. Most people with hepatocellular carcinoma have many small clusters of cancer cells called nodules. Some people have only one tumor that gets larger over time. Learn more about rare forms of liver cancer.
We encourage adults living with Hepatocellular Carcinoma to visit our Clinical Trials page to learn more about opportunities in the area. Visit the Clinical Trials page today.
Facts at-a-Glance
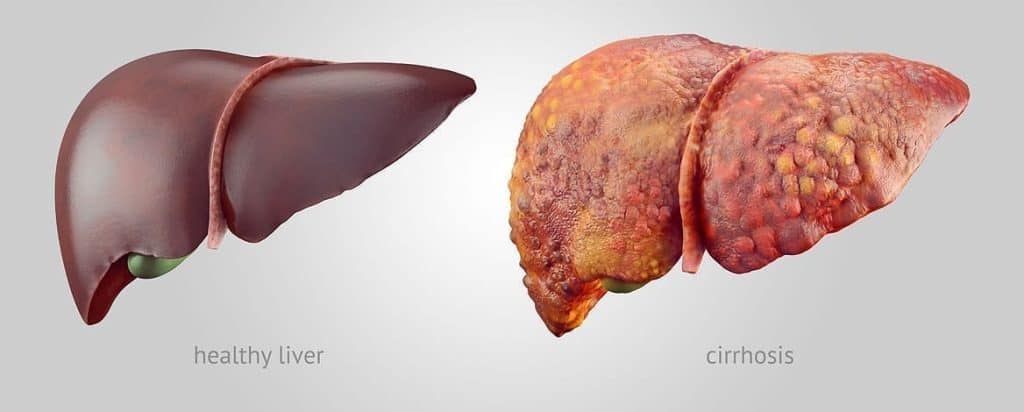
Liver disease is a progression that follows stages of illness. Some people with liver disease progress to cirrhosis (scarring) of the liver, which puts them at increased risk for liver cancer.
Liver cancer is more common among men than women.
The most current data indicates that liver cancer is among the top ten causes of death in the USA among all races, ethnicities, and genders. (Centers for Disease Control and Prevention, 2017) It claims the lives of approximately 34,000 Americans each year.
Liver cancer may have genetic or hereditary causes that are outside of our control. We may, however, be able to reduce our risk for developing liver cancer by being aware of the most common causes.
There are treatment options for people with liver cancer. Doctors suggest treatments based on type of cancer present, stage of cancer, and other information obtained through medical test results.
Risk Factors
A risk factor is something that increases the possibility of developing a disease. Certain conditions or behaviors can increase a person’s chances of developing liver cancer. Having cirrhosis is a risk factor for developing hepatocellular carcinoma (primary liver cancer). Cirrhosis is severe scarring of the liver due to a progression of damage to the liver, usually over many years. People often think that overuse of alcohol is the only way that cirrhosis can occur. In fact, drinking alcohol in excess is only one way in which a person can get cirrhosis.
Long-term (chronic) hepatitis B and hepatitis C infections are linked to hepatocellular carcinoma or liver cancer because they often lead to cirrhosis if they are undiagnosed and/or untreated. Hepatitis B is an exception to the norm in that it can lead to liver cancer without first causing cirrhosis in the progression of liver damage.
People with steatotic liver* may over time develop complications including cirrhosis, thereby putting them at risk for hepatocellular carcinoma or liver cancer. Certain conditions increase one’s chances of having fatty liver, including obesity, type 2 diabetes, high cholesterol, and high triglycerides.
People with certain hereditary and/or rare diseases may be prone to developing hepatocellular carcinoma or liver cancer. These include:
- Wilson Disease
- Alpha-1 antitrypsin deficiency
- Hemochromatosis
- Glycogen storage disease
- Advanced PBC
- Porphyria cutanea tarda
- Tyrosinemia
Environmental exposure to aflatoxins (poisonous cancer-causing agents produced by molds that grow in soil, decaying vegetation, hay, and grains) may lead to hepatocellular carcinoma.
Finally, long-term use of anabolic steroids has been linked to the development of hepatocellular carcinoma in some people.
People with any risk factor, or those who have been diagnosed with cirrhosis, should speak with their doctors about cancer screening and surveillance so that should cancer develop, it may be diagnosed sooner rather than later.
Reducing Your Risk
Understanding the risk factors for liver cancer is a big step in reducing your chances of getting liver cancer.
If you have a known liver disease, it is important to make and keep regular appointments with a medical provider who specializes in this field. Liver specialists are called gastroenterologists or hepatologists. You can still go to your primary care provider for your overall care and see the specialist for your liver care. If you are diagnosed with hepatocellular carcinoma, you will be referred to a liver cancer specialist. This type of specialist is called an oncologist.
Key steps you can take to keep your risk for liver cancer low include:
- Preventing exposure to hepatitis B (through blood and body fluids) and speaking to your doctor about getting the hepatitis B vaccine
- Preventing exposure to hepatitis C (through blood) from other people who may be infected (there is no vaccine for hepatitis C, but there is a treatment for people who are infected)
- Getting tested for hepatitis B and C if you may have been exposed
- Getting treatment for hepatitis B and/or C if you are infected
- Discussing your liver cancer risk with your doctor if you have other risks such as obesity, type 2 diabetes, high cholesterol, or if you drink heavily
Remember—people with cirrhosis should speak to their doctors about recommendations for regular surveillance and screenings for liver cancer. This can help detect cancer before symptoms start and the cancer becomes advanced.
Symptoms of Hepatocellular Carcinoma
People may not feel ill in the earliest stages of liver cancer, which is why it is very important to understand your risks and to talk to your doctor about liver cancer before you experience symptoms.
Once symptoms occur, they can include:
- Fatigue
- Bloating or feelings of fullness
- Pain on the right side of the upper abdomen or back and shoulder
- Nausea
- Loss of appetite
- Weight loss
- Weakness
- Fever
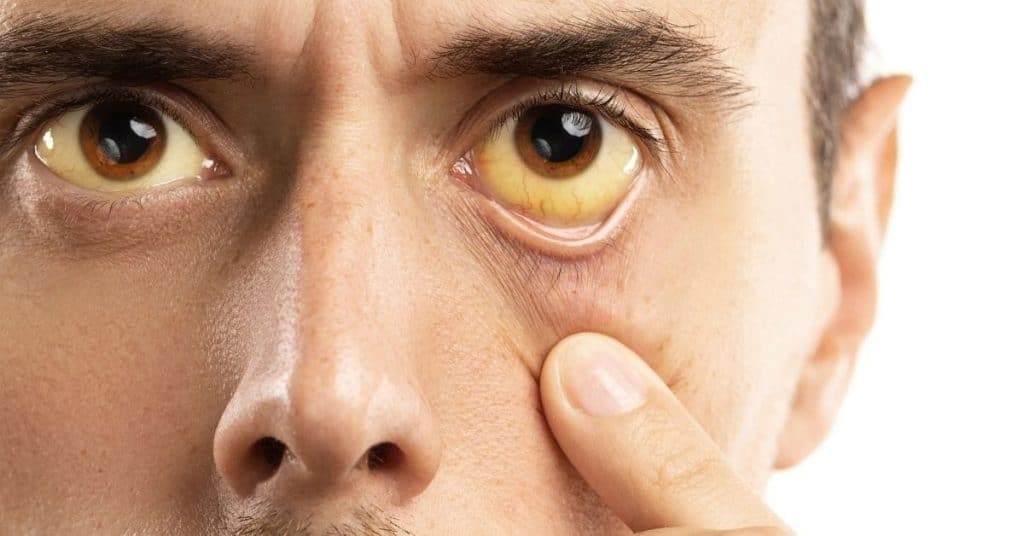
- Jaundice (yellowing of the skin and the whites of the eyes)
Diagnosis

Liver cancer is diagnosed through a physical examination and special medical tests. Diagnosis may include ultrasounds, CT scans, and MRI. Sometimes doctors may perform a liver biopsy, a procedure in which a small piece of liver tissue is removed and studied to confirm the diagnosis of liver cancer. Doctors may often do genetic testing of the cancer to help determine the best type of treatment for the patient.
Treatment
Liver cancer treatment depends on:
- The liver’s condition and the extent of cirrhosis
- The size, location, and number of tumors
- Whether the cancer has spread outside the liver or has remained within the liver
- The overall health of the patient and other risk factors for liver cancer

If the cancer has not spread and the rest of the liver is healthy, treatment options may include:
- Transplant (replacement of the liver)
- Partial hepatectomy or segmentectomy (surgery to remove a part of the liver or to remove a tumor from the liver)
- Radiofrequency ablation (inserting a thin probe through the skin and into the tumor to heat and destroy the cancer cells)
Sometimes the cancer may be contained within the liver but is not responsive to the above treatments. If this is the case, other treatments may include:
- Bland embolization, chemoembolization, or radioembolization of the blood vessels near the tumor (procedures to block the blood supply to the tumor, either with or without the use of anti-cancer medications)
- Radiation therapy (high-energy x-rays) to destroy cancer cells.
If the cancer has spread outside of the liver, or if it is still within the liver but not responsive to any of the above treatments, doctors may recommend some of the following treatments (either separately or in combination):
- Oral (by mouth) anti-cancer medications
- Immunotherapy (a type of treatment that helps your immune system fight cancer)
- Clinical trials (scientific studies to test new medications not yet available to the public
A successful liver transplant, also called a surgical resection, can cure liver cancer, but it is an option for only a small percentage of patients. Surgical resections are successful in only about one out of three cases. However, scientists are experimenting with several promising new treatments that could help prolong the lives of people with liver cancer.
Learn how the Liver Cancer Program at the National Institutes of Health, National Cancer Institute's Center for Cancer Research can help all liver cancer patients. This video features Tim Greten, MD, Co-Director of the NCI CCR Liver Cancer Program who provides information on clinical trials, liver cancer treatments and advice for patients.
Questions to Ask Your Doctor

If you have been diagnosed with hepatocellular carcinoma or liver cancer, you may feel shocked and scared. This is understandable. You will want to get as much information as you can from your doctor so that you will understand what is going on. Here are some questions that you can ask when you have your appointment.
- Do I have primary or secondary liver cancer?
- How many tumors do I have?
- What size are these tumors?
- Are there other tests I will need such as biopsy, imaging scans or PET scans?
- Has the cancer remained in the liver or has it spread?
- What treatment options do I have?
- Will I have to stay in the hospital for my treatments?
- What can be done to relieve my symptoms from the cancer?
- How effective is the treatment for liver cancer?
- What are the side effects of the treatment?
- Is it possible for my tumors to return after I finish treatment?
- Would I benefit from participation in a clinical trial? If so, where can I find more information about trials?
- Is liver transplant a possibility for me?
- Should I change my diet before and during treatment? If so, what should I eat? What should I avoid?
- Are there any supplements or medications that I should take or avoid?
- Can you recommend any support groups for me, my caregivers, and my family?
*Steatotic liver disease is the new name for fatty liver disease.
Patient Stories
Video Library
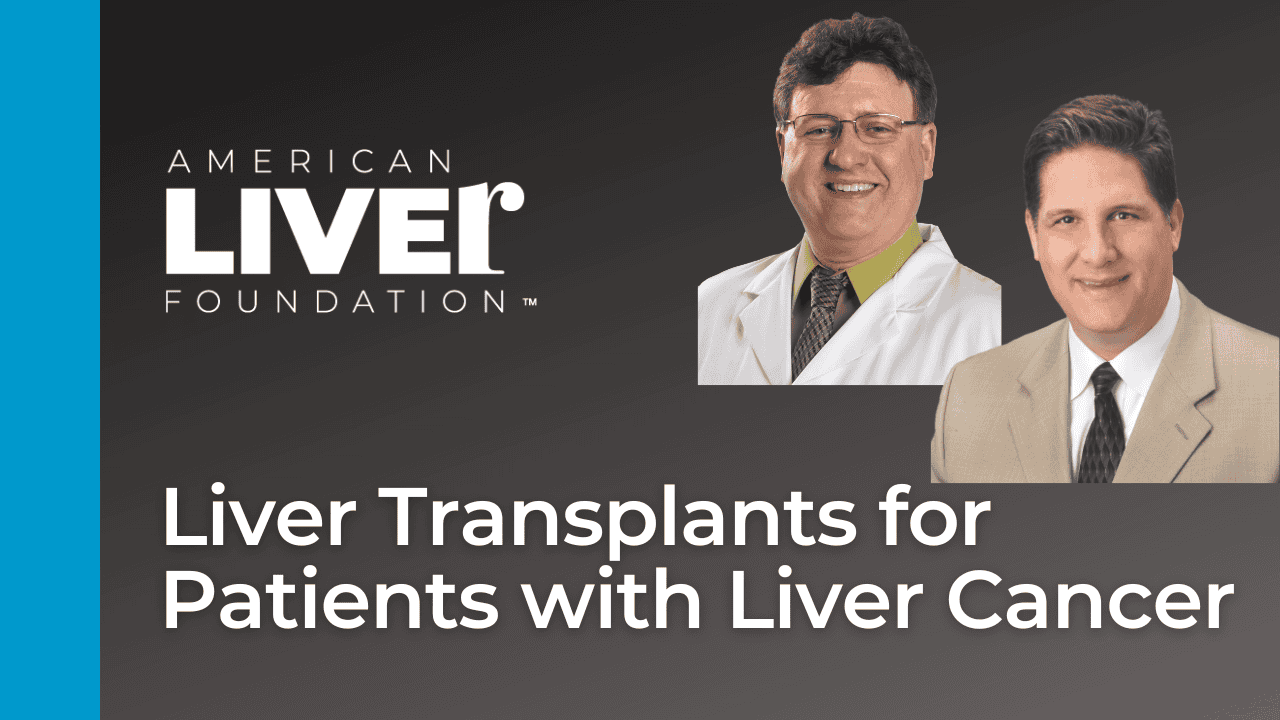
Register for an on-demand webinar
Watch a panel of liver cancer specialists from Memorial Sloan Kettering in a 1-hour on-demand webinar on new and emerging treatments for liver cancer. You will gain a better understanding of how those therapies work and which patients are most likely to benefit from which therapies. Learn about strategies to help with treatment-associated side effects. Learn how to be an advocate for better care and use support resources.
Register to watch anytime on demand now
Additional Resources and Information
Learn more about rare forms of liver cancer, including cholangiocarcinoma, fibrolamellar carcinoma, hepatoblastoma, and angiosarcoma.
Search for a Clinical Trial
Clinical trials are research studies that test how well new medical approaches work in people. Before an experimental treatment can be tested on human subjects in a clinical trial, it must have shown benefit in laboratory testing or animal research studies. The most promising treatments are then moved into clinical trials, with the goal of identifying new ways to safely and effectively prevent, screen for, diagnose, or treat a disease.
Speak with your doctor about the ongoing progress and results of these trials to get the most up-to-date information on new treatments. Participating in a clinical trial is a great way to contribute to curing, preventing and treating liver disease and its complications.
Start your search here to find clinical trials that need people like you.
*Steatotic liver disease is the new name for fatty liver disease.
Medically reviewed on April 2025.
Last updated on June 12th, 2025 at 12:33 pm